What are uterine fibroids?
Uterine fibroids (also called leiomyomas) are growths made of muscle and tissue that form in or on the wall of your uterus. These growths are usually not cancerous (benign) and are the most common noncancerous tumor in females.
Uterine fibroids can cause a variety of symptoms like pain and heavy, irregular vaginal bleeding. Sometimes, a person has no symptoms and is unaware they have fibroids. Treatment for fibroids typically depends on your symptoms.
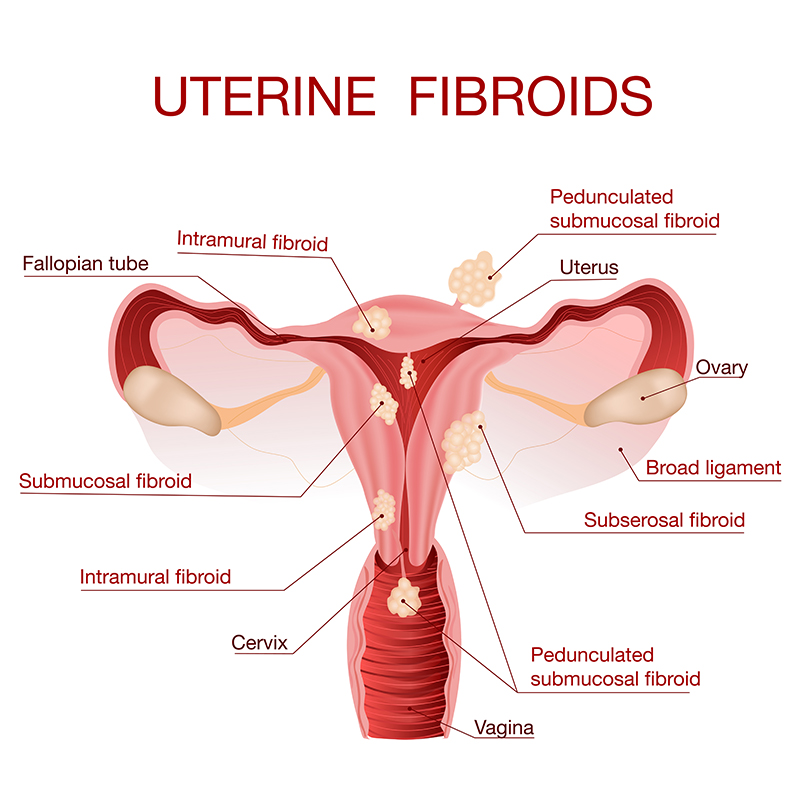
Where do fibroids grow?
Fibroids can grow as a single nodule (one growth) or in a cluster. Clusters of fibroids can range in size from 1 millimeter to more than 20 centimeters (8 inches) in diameter or even larger. For comparison, fibroids can be as small as a seed or get as large as a watermelon. These growths can develop within the wall of your uterus, inside the main cavity of your uterus or on the outer surface of your uterus.
Types of uterine fibroids
There are different types of uterine fibroids depending on where they’re located and how they attach. Specific types of uterine fibroids include:
- Intramural fibroids: These fibroids are embedded into the muscular wall of your uterus. They’re the most common type.
- Submucosal fibroids: These fibroids grow under the inner lining of your uterus.
- Subserosal fibroids: This type of fibroid grows under the lining of the outer surface of your uterus. They can become quite large and grow into your pelvis.
- Pedunculated fibroids: The least common type, these fibroids attach to your uterus with a stalk or stem. They’re often described as mushroom-like because they have a stalk and then a wider top.
Are fibroids common?
Fibroids are a very common type of growth. Approximately 40% to 80% of people with a uterus have fibroids. They occur most often in people between 30 and 50 years old. People who haven’t had their first period (menstruation) yet typically don’t have fibroids. They’re also less common in people who’ve entered menopause.
Symptoms and Causes
What are uterine fibroids and what are the risk factors?
What are the symptoms of uterine fibroids?
Most small fibroids don’t cause any symptoms and don’t require treatment other than regular observation by your healthcare provider. Larger fibroids can cause you to experience a variety of symptoms, including:
- Excessive or painful bleeding during your period.
- Bleeding between your periods.
- A feeling of fullness in your lower belly (abdomen)/bloating.
- Frequent urination (this can happen when a fibroid puts pressure on your bladder).
- Pain during sex.
- Low back pain.
- Constipation or feeling pressure on your rectum.
- Long-term (chronic) vaginal discharge.
- Inability to pee or completely empty your bladder.
- Increased abdominal distention (enlargement), causing your abdomen to look pregnant.
The symptoms of uterine fibroids usually stabilize or go away after you’ve gone through menopause because hormone levels decline within your body.
What does uterine fibroid pain feel like?
There are a variety of feelings you might experience if you have fibroids. If you have small fibroids, you may feel nothing at all and not even notice they’re there. For larger fibroids, however, you can experience discomfort and pain. Fibroids can cause you to feel back pain, stabbing pains in your abdomen and even pain during sex.
What do fibroids look like?
Fibroids are typically rounded growths that look like smooth bumps. In some cases, they can be attached with a thin stem, giving them a mushroom-like appearance.
What causes uterine fibroids?
The exact cause is unknown, but healthcare providers believe the hormones estrogen and progesterone play a role. Most fibroids happen in people of reproductive age. Studies show that fibroids tend to grow when hormone levels are higher (like during pregnancy) and shrink when hormone levels are low (like during the transition to menopause).
What are risk factors for uterine fibroids?
There are several risk factors that can play a role in your chances of developing fibroids. These can include:
- Obesity and a higher body mass index (BMI).
- Family history of fibroids.
- Not having children.
- Early onset of menstruation (getting your period at a young age).
- Late age for menopause.